Abstract
CD4+CD25+FOXP3+ regulatory T cells (Treg) are dominant suppressors of innate and adaptive immune effector cells that enhance tolerance. Treg augmentation can control immune activation underlying chronic graft-versus-host disease (cGVHD). In prior studies, daily subcutaneous (SC) low-dose interleukin-2 (IL-2) therapy for 8-12 weeks induced preferential Treg expansion in-vivo, with objective clinical responses in over half of evaluable participants (NEJM 2011, Blood 2016). Alternative immunomodulatory approaches like extra-corporeal photopheresis (ECP) also have efficacy in cGVHD and may function via Treg augmentation. Combining ECP plus IL-2 could offer therapeutic synergy.
We report on a prospective single arm phase 2 trial of twice-weekly ECP (weeks 1-16) plus sequential low-dose IL-2 (1x106 IU/m2/d SC, weeks 9-16) for treatment of steroid-refractory cGVHD. The study enrolled 25 participants (48% male, 88% HLA-matched, 100% PBSC grafts, 52% prior aGVHD). Median participant age was 62 years (range, 34-76). Median time from HSCT and from cGVHD onset to start of treatment was 919 days (range, 177-2842) and 524 days (range, 58-2697) respectively. Participants had a median of 3 cGVHD organ sites (range, 2-5). The median follow-up time in survivors is 16 months (range, 2.1-26).
ECP plus IL-2 was well tolerated: 1 participant withdrew due to IL-2 adverse effects (AE) (myalgia, fatigue), and 3 were additionally unevaluable (1 cardiac arrest; 1 parainfluenza infection, 1 still undergoing treatment). None required IL-2 dose reduction. There were four grade 3 AEs during the 16-week study (1 participant had dehydration/hypotension/syncope, possibly IL-2-related;1 had ECP-related anemia). None experienced relapse. At week 16, cGVHD objective partial responses (PR) were documented in 14 of 21 evaluable participants (67%). None had cGVHD progression. Response sites included skin (n=9/18), joint/fascia/muscle (n=7/16), liver (n=1/1), lung (n=2/9), and GI tract (n=3/5). 18 participants with clinical benefit (PR, and stable disease with minor response) proceeded to extended ECP plus IL-2 therapy.
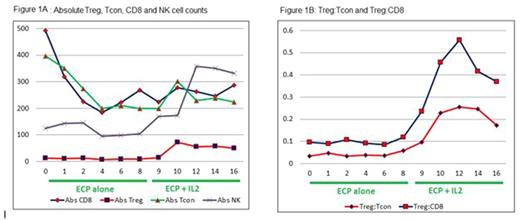
Immunologically, 8 weeks of ECP alone did not induce significant changes in buffy coat WBC or absolute lymphocyte count (ALC). Peripheral blood CD3 T cell counts/µL fell, with a median CD8 and CD4 conventional T cell (Tcon) decrement of -109 (Q1, Q3: -220, -13; p<0.001) and -68 (Q1, Q3: -244, -19; p=0.023), respectively, at week 8 (Figure 1A). There was an early fall in Treg cell counts/µL, with a median decrement of -4 (Q1, Q3: -9, 0; p=0.033) at week 4, without change in NK or B cell counts or Treg:Tcon ratio. The addition of low-dose IL-2 thereafter induced a >5-fold increase in median Treg count/µL (p<0.001), from a baseline of 9 (Q1, Q3: 5, 17) at week 8 to a peak of 72 (Q1, Q3: 22, 186) at week 10, plateauing at 50 (Q1, Q3: 33, 71) at week 16 (Figure 1A). No significant change in CD4 Tcon or B cell count was noted. NK cell count increased 1.7-fold (p=0.009). The median Treg:Tcon ratio increased 4-fold (p<0.001): from a baseline of 0.06 (Q1, Q3: 0.03, 0.08) at week 8 to a peak of 0.26 (Q1, Q3: 0.12, 0.42) at week 12, and remained elevated at 0.17 (Q1, Q3: 0.14, 0.34) at week 16 (Figure 1B). Treg count and Treg:Tcon ratio remained elevated in responders during extended ECP plus IL-2 therapy.
Immunologically, clinical responders had a higher median Treg count/µL vs. non-responders after 1 and 6 weeks of IL-2 therapy (21 vs. 11, p<0.001; 73 vs. 29, p=0.016 respectively). Treg:Tcon ratio at week 2 and 6 after IL-2 therapy was also higher in responders (0.29 vs. 0.15, p=0.038; 0.28 vs. 0.13, p=0.016 respectively). Applying our previous cutoffs (Blood 2016), Treg:Tcon ratio ≥0.2 after 1 week of IL-2 was also predictive of clinical response (p=0.05).
In summary, in steroid-refractory cGVHD, ECP was associated with a fall in peripheral CD8, CD4 Tcon, and Treg counts. The addition of low-dose IL-2 thereafter induced profound Treg and NK cell augmentation. Clinical responses (PR) to combination ECP plus IL-2 therapy were documented in 67% of the evaluable participants. Those with early rise in Treg count and Treg:Tcon ratio after the addition of IL-2 were likelier to benefit. However, the overall clinical efficacy of ECP plus IL-2 did not appear markedly higher than low-dose IL-2 alone.
Koreth: Prometheus Labs: Research Funding; Kadmon Corp: Membership on an entity's Board of Directors or advisory committees; Millennium Pharmaceuticals: Research Funding; Takeda Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Amgen Inc.: Consultancy. Armand: Bristol-Myers Squibb: Consultancy, Research Funding; Merck & Co., Inc.: Consultancy, Research Funding; Sequenta/Adaptive: Research Funding; Sigma Tau: Research Funding; Tensha: Research Funding; Affimed: Research Funding; Roche: Research Funding; Pfizer: Consultancy, Research Funding; Genmab: Consultancy; Infinity: Consultancy; Otsuka: Research Funding. Antin: Gentium SpA/Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal